Does SASH Really Work?
From July 2011 to June 2015, SASH participants realized an average savings of $1,227 per person per year in Medicare expenditures.
From the "Better Care, Healthier People, Smarter Spending" Report, April 2018.
Here is a sampling of SASH success stories during the COVID-19 pandemic.
As the coronavirus arrived in Vermont, SASH coordinators and wellness nurses were contacting every participant to design an individual action plan for COVID-19. During one such call, the nurse discovered that a diabetic participant had a painful foot ulcer. She had not sought treatment for fear of contracting the virus. The resident-services manager at Copley Terrace reached out to SASH seeking help for a resident who could no longer shop for groceries due to the shutdown of the community transportation service. The out-of-state son of a SASH participant called the SASH coordinator after becoming concerned about his mother. He had talked to her several times that weekend and said she was confused. He wanted to call an ambulance and have her evaluated at the hospital. As the conversation continued, the SASH coordinator suspected there might be a problem with a recent medication change and convinced the son to hold off. A SASH participant whose wife had died a year ago experienced a delayed and traumatic grief response during the early weeks of the pandemic. He had always prided himself on never needing help, but the isolation brought on by the pandemic caused buried feelings to rise to the surface. He acknowledged his severe distress at the end of a casual conversation with the SASH coordinator, who quickly connected him with the SASH wellness nurse. A worker from the local crisis hotline reached out to the SASH coordinator about a participant who was experiencing high levels of stress, anxiety and loneliness related to COVID-19 isolation. The SASH coordinator immediately contacted the individual by phone. She learned that the participant was physically okay but potentially at risk for suicide. The SASH coordinator and wellness nurse contacted local partners and quickly arranged for mental health wrap-around services through local agencies. The person is now stabilized and reportedly is doing well.
After further conversation, the nurse determined immediate medical attention was required. The nurse convinced the woman she needed treatment and then made the appointment for her. Without SASH’s intervention, the ulcer likely would have worsened, which could have led to hospitalization, surgery and/or amputation, as well as costly follow-up care.
Upon learning that the resident had no local family or other supports to draw upon, the SASH Coordinator jumped into action, ensuring that the participant had essential groceries until the local transportation service was restored. The SASH coordinator continues to follow up weekly with this person.
The SASH coordinator gathered initial information and connected with the SASH wellness nurse. The nurse accessed the participant’s medical records online and then contacted the pharmacist of record, whose information did not match what was in the participant’s medical records.
The nurse contacted the office of every medical provider and was able to compile an accurate medication list. She coordinated with numerous family members to inform them of the woman’s current (and correct) medications, then donned appropriate PPE and conducted a home visit with the participant, interacting with her from the porch.
She verified that the woman’s pillbox was correctly filled for the week and determined that unclear communication from health care providers was the cause of her confusion. Daily follow-up with the participant confirmed that she was taking her medications properly and was no longer confused.
Thus, SASH helped the participant and the family and made it possible to avoid an expensive and unnecessary trip to the hospital and potential hospitalization.
Their weekly, supportive conversations continue to this day. No longer distraught, the participant recently told the SASH coordinator that if it wasn’t for SASH, he would not be here.
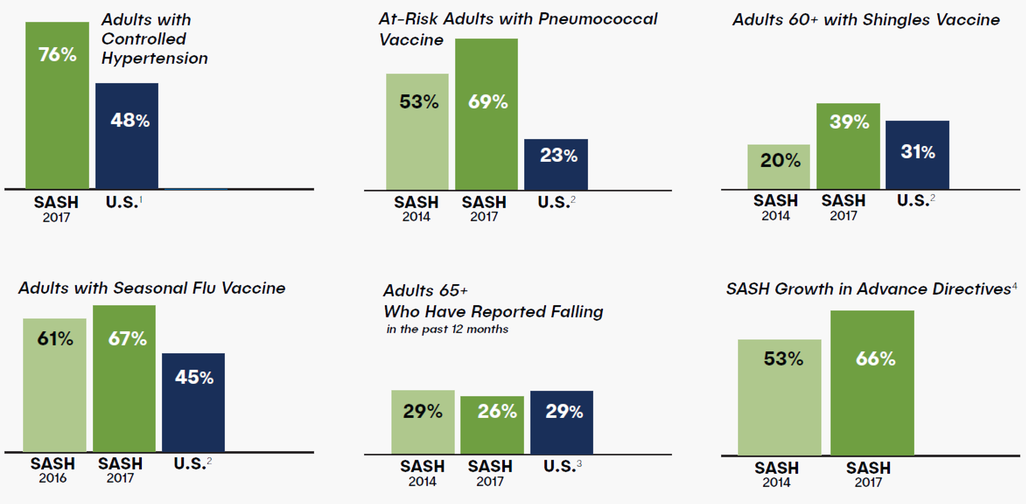
Since its inception in 2012, SASH has shown tremendous improvements in the well-being of its participants, with results that outperform the national average. According to a 2018 report on the impact the SASH program has had, SASH participants realized an average savings of $1,227 per person per year in Medicare expenditures. In addition, a study published in the Journal of the American Medical Association indicates that "3,300 SASH participants with advance directives could translate into a savings of $18.4 million in end-of-life care.”
 1) cdc.gov/mmwr/volumes/66/wr/mm6632a3.htm#F1_down
1) cdc.gov/mmwr/volumes/66/wr/mm6632a3.htm#F1_down
2) cdc.gov/mmwr/volumes/66/ss/pdfs/ss6611.pdf
3) cdc.gov/mmwr/volumes/65/wr/mm6537a2.htm
4) Analysis of statewide SASH data
* Highlights of the First Four Years of SASH (summary of four-year evaluation), U.S. Dept. of Health & Human Services, Assistant Secretary for Planning and Evaluation: aspe.hhs.gov/pdf-report/support-and-services-home-sash-evaluation-highlights-first-four-years-research-summary
** Journal of the American Medical Assn., 2011 Oct 5; 306(13):1447-53. doi: 10.1001/jama.2011.1410. Regional variation in the association between advance directives and end-of-life Medicare expenditures; cites $5,585 savings per decedent in Vermont’s 2 Hospital Referral Regions.

